What does pancreas do?
|
What is acute pancreatitis?
Acute pancreatitis is an inflammation of the pancreas that occurs suddenly. It differs from chronic pancreatitis in that there is a discrete episode.
Acute pancreatitis which may be classified as mild, moderate or severe, depending on the amount of damage and organ dysfunction caused by the pancreatitis.
What are causes or risk factor of acute pancreatitis?
Causes of acute pancreatitis are :
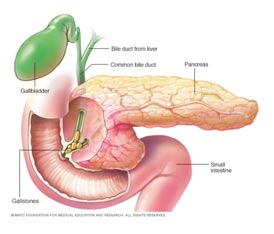
- Biliary stones are the cause of 35 to 50 percent of the cases of acute pancreatitis.
- Alcohol intake is the second leading cause of acute pancreatitis.
- Several drugs may cause pancreatitis e.g, immunosuppressants, estrogens, acetaminophen, sulindac. tetracycline, salicylates, erythromycin, pentamidine, thiazide diuretics, furosemide and valproic acid.
- Viral causes include hepatitis A, B, and non-A/non-B; cytomegalovirus; mumps; and coxsackievirus.
- Bacterial causes may include Legionella, mycoplasma and mycobacterium tuberculosis.
- Parasitic infections may also cause acute pancreatitis.
- Pancreas divisum (a congenital defect of the pancreatic ducts).
- Metabolic imbalances (hyperlipidemia and hypercalcemia).
- Sphincter of Oddi dysfunction.
- Scorpion stings.
- Trauma to pancreas may also cause acute pancreatitis.
What are symptoms of acute pancreatitis?
- Upper abdominal pain is main symptom. Usually it is severe and radiates to back.
- Nausea and vomiting are the other most frequent symptoms of acute pancreatitis.
- Fever
- High pulse rate.
- Few patients may have jaundice.
- Patient may have low blood pressure and confusion or coma may occur.
Can acute pancreatitis become chronic pancreatitis?
Yes. Chronic pancreatitis results when inflammation in the pancreas has caused damage and resulted in fibrosis, calcifications and ductal inflammation. It is also possible for patients with chronic pancreatitis to have episodes of acute pancreatitis. Chronic pancreatitis is slow self propagating disease that results in slow destruction of pancreas.
How is acute pancreatitis diagnosed?
Diagnosis of acute pancreatitis is usually made clinically when patient presents with typical pain of pancreatic origin that is pain upper abdomen radiating to back. Further tests helps in confirming diagnosis e.g,
- Increased serum amylase and/or lipase (pancreatic enzymes).
- Ultrasound abdomen
- CT Scan abdomen
Can I prevent acute pancreatitis?
Avoidance of known causes of pancreatitis (i.e., alcohol consumption) may help prevent the onset of the disease. Lifestyle factors such as obesity, alcoholism, hepatitis and others that contribute to a poor state of overall health lead to complications of acute pancreatitis and to a poorer prognosis for recovery.
What is treatment of acute pancreatitis?
The treatment of acute pancreatitis depends on its severity.
- If the disease is considered mild, the patient is usually treated supportively with intravenous fluids, pain control medication, keeping close watch on patient’s general condition so that it does not deteriorates.
- Severe pancreatitis requires close monitoring of the patient to detect possible systemic complications. The patient may be admitted to an intensive care unit. Organisms may reach the pancreas and infect it by crossing the colonic wall. Antibiotics may be used to prevent sepsis. These patients may have some organ failure thus require support for these failed systems.
- Surgical debridement and drainage may be necessary if infected pancreatic necrosis (cell death) arises. CT scan-guided aspiration of necrotic areas may be done to identify the infecting organism so that it may be treated effectively. Surgical intervention is usually done 4 weeks after onset of pancreatitis.
- Therapeutic endoscopic retrograde cholangiopancreatography (ERCP) may be performed in the early stages of acute pancreatitis to remove gallstones and may require sphincterotomy (cutting the sphincter muscle to allow drainage from the biliary/pancreatic tract).
What are possible complications of acute pancreatitis?
Complications can be localized or systemic.
- Systemic complications are usually seen in severe acute pancreatitis. These include
- Low blood pressure
- Lung failure
- Kidney failure
- Inflammation may extend to surrounding organs such as the colon and stomach, gastrointestinal bleeding.
- Localized complications include
- Fluid collections
- Pancreatic pseudocysts
- Pancreatic necrosis
- Pancreatic abscess
Is there hereditary link with acute pancreatitis?
No. There may, however, be genetic influence in chronic pancreatitis.

 Book An Appointment
Book An Appointment