Liver Cancer Treatment Surgery Chandigarh
What are the symptoms of liver cancer?
Symptoms of liver cancer vary widely and may include
What are the risk factors for liver cancer?
- Viral hepatitis such as hepatitis B and C
- Regular alcohol consumption
- Cirrhosis – cirrhosis due to any cause increases the risk of liver cancer
- Diabetes – It can result in fatty liver disease and thus leading to hepatitis and predisposes to cancer.
- Non alcoholic fatty liver disease – it can lead to inflammation of liver cell thus predisposing to formation of cancer.
- Hereditary conditions like hemochromatosis( iron deposition in liver), Wilson disease ( copper deposition in liver)
- Aflatoxins – consumption of food product infected with fungus producing aflatoxins can also produce liver cancer
How can liver cancer be prevented?
Prevention is very important when it comes to a disease like liver cancer. The underlying cause of liver cancer is often liver inflammation and the development of a condition called Cirrhosis. In addition to avoidance of drugs and alcohol, infection (such as Hepatitis B or C) and obesity can contribute to the development of liver cancer.
Steps to minimize these risks include
- Vaccination against hepatitis B for those at risk,
- Prompt treatment for patients infected with hepatitis C,
- Maintaining a healthy weight through diet and exercise.
- Avoidance of alcohol
- Good control of diabetes.
How is liver cancer detected?
Patients diagnosed at an earlier stage have better outcomes. There are many strategies that are used to detect liver cancer, including.
Several researchers are looking to find the one blood test that will help identify liver cancer much sooner. Until that time, we continue to remain vigilant and screen with a variety of methods to try to catch this disease as early as possible.
Are fatty liver disease and liver cancer related?
Fatty liver disease progressing onto non-alcoholic fatty liver disease(NAFLD) and non-alcoholic steatohepatitis(NASH) can result in cirrhosis of the liver. Cirrhosis of the liver predisposes the patient to liver cancer. The fatty liver itself does not predispose a patient to cancer however if it is controlled at an early stage before it progresses onto cirrhosis then the risk of liver cancer is negligible.
What is the optimal treatment of liver cancers?
In general, the basic approach of any cancer therapy can also apply to liver cancer. The treatment of the local disease. In liver cancer, we often address the local disease with:
without cirrhosis of the liver.
cirrhosis provided tumor size and number criteria are met. It takes
care of cirrhosis of the liver also.
Are herbal medicines recommended to treat liver cancer?
The term ‘herbal medicine’ can represent thousands of compounds. Unfortunately, most are not rigorously tested or regulated by the companies that produce them, so real evidence of any benefit is not known. In fact, they may have harmful side effects that one comes to know only after using them.
Should I be worried if I have a cyst on my liver?
There is often nothing to worry about with simple cysts in the liver. They can be quite common. When we find cysts that are growing, we will often take extra care to ensure that
- There is not an associated tumor causing the growth
- That cyst is not causing problems.
This is often discussed over time with your hepatologist and/or liver surgeon who can help in differentiating malignant ( cancerous) cysts from nonmalignant ones.
What should I do if some lesion is found in the liver on a regular check-up?
Lesions in the liver on ultrasound can be of many types
Non-cancerous
- Hemangioma ( abnormal formation of blood vessels)
- Abscess ( pus collection in liver)
- Granulomas in liver- because of TB , Sarcoidosis etc.
- Cysts of liver – that can be simple cyst or hydatid cysts ( worm infestation)
Cancerous
- Primary liver cancer
- Metastatic tumor from some other organ- liver is most common site of spread of tumors from other abdominal organs.
- Neuroendocrine tumor of liver
- Malignant cysts of liver
A hepatologist or liver surgeon can help you in guiding you towards diagnosis and treatment by carrying out relevant investigations.
If a parent had/has liver cancer, are their children at greater risk of getting it?
In some cases, yes, a parent with liver cancer can raise your personal risk e.g in hereditary disease as Hemochromatosis, or Wilson’s disease. However, this is not true for the majority of patients. It’s always good to talk to your primary care doctor about your concerns or questions.
Gall Bladder Stone Treatment in Chandigarh Mohali
Gall bladder diseases are very common these days. These diseases range from innocuous gall stones to cancer of the gall bladder which has a very dismal prognosis. As a GASTROINTESTINAL SURGEON with HEPATOBILIARY experience we daily see cases from one extreme to another. The majority are simple gall stones and are managed at the periphery, however, what we receive are ones that are either left to be referred to as higher-level or are complicated ones. Many a times we also deal with cases that are operated elsewhere and become complicated and are then referred to us.
So today in this blog I would like to discuss gall bladder diseases with a special focus on stone diseases. The most commonly asked questions in the patient’s mind are
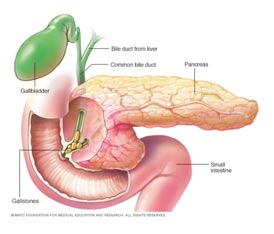
How are stones formed?
Bile is juice produced by the liver and stored in the gall bladder and released when food reaches the small intestine. It is composed of bile salts, and pigments, and they are kept in solution form by mixing with cholesterol. So any change that disturbs this proportion of each component required to keep these in solution form can result in the formation of stones. For example diet rich in fats can result in high cholesterol components and can result in stone formation.
How can we prevent formation of gall stones?
Gall stones are usually formed by a mismatch in the concentration of cholesterol and bile salts in bile. So a balanced diet that is low in fats can help in decreasing the chances of gall stone formation.
What are risks associated with gall stones?
Gall stones can cause pain by themselves. They can result in jaundice if a stone slips into bile duct. It can cause pancreatitis which can be mild or life-threatening. The gall bladder neck can be blocked by stone resulting in huge distension of the gall bladder thus causing pain and can result in pus formation in the gall bladder. Large stones in gall bladder are risk factors for cancer of gall bladder.
If they are not causing any trouble, should I undergo surgery?
These are called asymptomatic stones. Asymptomatic stones usually do not require surgery unless
a. Patient is having low immunity
b. The patient is living in a place where medical facilities are meager.
c. Patient is undergoing surgery of abdomen for some other reason
Relative indications are
i. Multiple small stones
ii. Diabetic patient
iii. Large stone
Can we just remove stones and leave gall bladder behind?
We have to remove the gall bladder as its functionally abnormal and stones would reform. Moreover cut on gall bladder heal very poorly.
Will removal of the gall bladder affect my digestion?
There is no effect on digestion if the gall bladder is removed. Body adapts to removal of gall bladder very well and digestion is not affected at all.
What are dietary restrictions after gall bladder surgery?
There is no dietary restriction and the patient can have a normal diet as before. Digestive system adapts well to removal of gall bladder and there is no effect on the digestion of food.
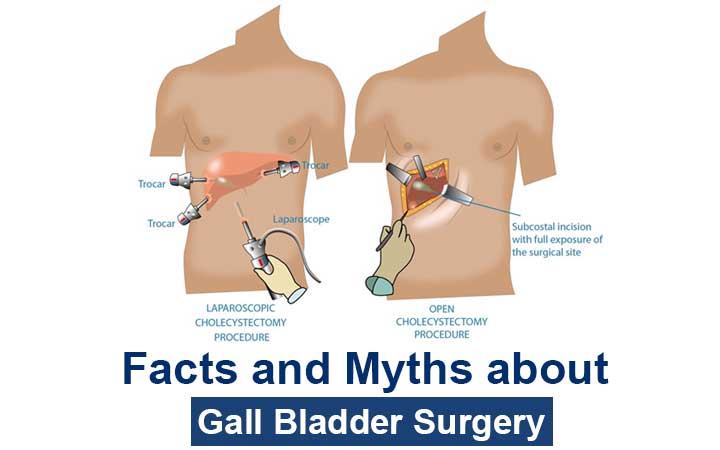
Is it major surgery?
Gall bladder removal surgery is performed by laparoscopy. It is successful in more than 99% of cases. Occasionally it is done by open surgery if anatomy is difficult or there is a risk of injury to important structures. But as the experience of the surgeon increases chances of conversion to open procedure decrease.
Is it very painful?
Laparoscopy surgery is done through small cuts made on your tummy ranging from 0.5-1 cm. these are small cuts and pain is minimum.
Should we undergo open or laparoscopic surgery?
That is to be decided by the surgeon operating upon you. As mentioned above large majority of procedures can be done by laparoscopy and needs open surgery only if surgery is difficult or in the presence of gall bladder cancer.
How long does it take to remove gall bladder?
Surgery is never about time. It is better to finish the procedure safely than quickly. It may take from 10 mintues to an hour depending upon anatomy.
What are the risks of surgery?
Apart from anaesthesia risk that depends upon general condition of patient gall bladder surgery carries minimum risk. Still there is a small but real risk of bleeding, injury to bile duct or injury to bowel.
How long does it take to recover and get back to normal life?
Gall bladder surgery is usually done as daycare surgery and the patient is send home same evening of surgery. The patient is up about a Few hours after surgery and starts his normal routine within a few days of surgery.
How does the experience of the surgeon matter in gall bladder surgery?
The experienced surgeon has fewer conversion rate and the chances of complication are less. Surgeon experienced in hepatobiliary or gastrointestinal surgery can handle the majority of complications on table and can provide better outcome in difficult cases.
Why some people are unsatisfied after gall bladder surgery?
Gallstones can cause abdominal pain, bloating, or discomfort after food intake and the complications listed above. Symptoms such as indigestion, heartburn, constipation and increased frequency of stools are very common in the general population and are not related to gallstones. Mostly when the patients / treating doctors try to correlate these symptoms with gallstones it leads to unhappiness as these symptoms may not get relieved by the removal of the gall bladder. So proper patient selection and counseling can help avoid the unsatisfied patient.
Gall bladder Cancer
1. What are causes of gall bladder cancer?
Known causative factors for gall bladder cancer are
- Gall Stones
- Gall bladder Polyps
- Porclein gall bladder
- Obesity
- Old age
- Choledochal cyst
- Abnormalities of union of bile and pancreatic duct
- Primary sclerosing cholangitis
- Ethnicity
- People residing in high-risk area eg., Chile, along plains of river Ganges etc.
2. What are signs and symptoms of gall bladder cancer?
Gall bladder cancer can present with very non-specific signs and symptoms. Majority times it is
detected incidentally on imaging. Patient may present with
- Pain
- Jaundice
- Loss of weight
- Loss of appetite
- Distension of abdomen
3. How can gall bladder cancer be detected?
Gall bladder cancer usually are detected on imaging. Ultrasound abdomen is first lie of
investigation that can show irregular thickening of gall baldder wall. These findings are
confirmed by multiphasic CECT abdomen that can show condition of gall bladder and
surrounding enlarged lymph nodes.
4. Are gall bladder polyps cancerous?
Small gall bladder polyps are non cancerous. Any polyp larger than 1 cm in size harbour
higher chances of malignancy and is an indication of surgery.
5. How can gall bladder cancer be prevented?
Gall bladder cancer cannot be prevented . There are no ways by which gallbladder
cancer can be prevented except for prophylactic cholecystectomy in area of high endemicity eg., Chile ,
where prophylactic cholecystectomy had been shown to decrease incident of gall bladder
cancer.
6. What is treatment of gall bladder cancer?
Main treatment of gall bladder cancer is surgery is it is feasible. Complete resection of gall
bladder cancer is the only chance of providing long term survival. Usually majority of patients
present with advanced disease that cannot be resected and can be offered palliative treatment
only. Resectability if usually assessed best by liver/gastrointestinal surgeon who is experienced
in liver surgery. Assessment by liver surgeon can make advanced disease resectable by proper
planning with help of interventional radiologist. Chemotherapy has a role in pallative setting or
after resection of tumor by surgery.
Colon and Rectal Cancer
1. What is colon?
A colon, also called the large intestine or large bowel, is part of the body’s digestive system. The colon is a muscular tube about five feet long and three inches wide. During digestion, food moves from the stomach to the small intestine and then to the colon. The colon absorbs water and nutrients from the body’s waste, creates stool and then pushes that stool into the rectum.
2. What is the differences between colorectal, colon and rectal cancer?
Colorectal cancer is the term used to describe cancer of the colon and/or rectum. The two cancers are grouped together because they share many common characteristics. Together, the colon and rectum make up the large intestine, a question mark-shaped bowel four feet in length. Colon cancer develops in all but the last few inches of the large intestine, between the appendix and rectum. Rectal cancer develops in the rectum, the last few inches of the large intestine that attaches to the anus. Colon cancer is more common.
3. What are polyps?
A polyp is a clump of cells that forms on the lining of the colon giving rise to swelling that project from wall of colon into lumen of colon. Most polyps are not harmful, but some may develop into colon cancer. Colonoscopies can help detect pre-cancerous polyps
4. What are sign and symptoms of colon cancer?
Colorectal cancer may develop when benign polyps in the large intestine grow and become cancerous. If early-stage colorectal cancer does cause symptoms, early warning signs may include sudden weight loss and/or narrow, ribbon-like stools. Other common early warning signs of colorectal cancer include:
- Rectal bleeding, either bright or dark red in color
- Tenesmus, which is the feeling that you have to empty your bowel but nothing passes
- Anemia caused by iron deficiency
- Persistent abdominal pain
As the cancer grows, symptoms may include:
- Abdominal pain or cramps
- Constipation
- Diarrhea
- Blood in your stool
- Bloating or a sense of not feeling empty after a bowel movement
- Flat or ribbon-shaped stool
- Unexplained weight loss
- Fatigue
- Loss of appetite
5. What are risk factors for colon cancer?
A risk factor is something that increases your chances of getting a disease. Having a risk factor does not mean that you will definitely get a disease, only that you and your doctor should watch more carefully for warning signs. Some risk factors can be avoided through lifestyle changes and some cannot. Some of the risk factors for colon cancer include:
- Age 50 or older
- Type-II diabetes
- Personal or family history of colon cancer or polyps
- Personal history of inflammatory bowel disease
- Some inherited genetic syndromes
- Diet high in fat and/or low in fiber or calcium
- Obesity
- Smoking
- Heavy drinking
- Physical inactivity
6. How is colon cancer diagnosed?
Doctors use many tools and techniques to diagnose colon cancer including:
- History and physical examination by a physician
- Testing blood and stool
- Performing colonoscopies
- Performing CT scans, PET scans, MRIs, endoscopies, and ultrasounds
7. How can we prevent / decrease risk of colon cancer?
The risk factors for colorectal cancer may be reduced with regular checkups and lifestyle changes. In western countries it is recommended that men and women have a colonoscopy beginning at age 50 as the rates of cancer are higher in west. If you have a family history of colorectal cancer, you should get screened 10 years earlier than when your family member was diagnosed. For example, if your father was diagnosed with colon cancer at 48, you should talk to your doctor about getting a colonoscopy at 38. Talk to your doctor about how often you should get a colonoscopy. The procedure may be able to help your doctor spot cancer in its early stages. Pre-cancerous polyps are removed and biopsies are performed during the procedure, if necessary.
Changes in your lifestyle may also help you lower your risk and prevent colorectal cancer from developing. Obesity, smoking, alcohol, diet and a sedentary lifestyle have been linked to an increased risk for colorectal cancer
8. Is colon cancer hereditary?
Colorectal cancer isnt always passed down in families, but it can be. If someone in your family has had colorectal cancer, you may be more likely to develop it.
Colorectal cancer can sometimes be caused by Lynch syndrome, a genetic condition also called hereditary nonpolyposis colorectal cancer (HNPCC). About one in 30 colorectal cancer cases are a result of Lynch syndrome. Patients with Lynch syndrome tend to get colorectal cancer at a younger age than others, with a higher likelihood of developing other types of cancer as well, such as:
- Stomach cancer
- Liver Cancer
- Ovarian Cancer
- Uterine Cancer
9. How is colon cancer treated?
Surgery is the most common form of treatment for colorectal cancer. Surgery is used to remove the tumor and surrounding tissue. A portion of the colon or rectum may need to be removed, and a colostomy( part of colon is brought out through abdominal wall and bag if fixed over it in which stool gets collected) may be required—permanently or temporarily, depending on the extent of the cancer and how much of the colon or rectum is removed. Other treatment options include chemotherapy and/or targeted therapy drugs, which may also be used in addition to surgery. Radiation therapy is usually an option only for rectal cancer, not colon cancer.
10. What types of doctors will I see during my treatment?
Your colorectal cancer care team may include one or more of these doctors:
- A gastroenterologist, who specializes in the digestive system and performs colonoscopies
- Surgical gastroenterologist/ GastroIntestinal Surgeon – who performs surgery to remove tumors and provide best functional outcome e.g pouch formation in case of hereditary cancers. If disease is early only surgery can be curative.
- A radiation oncologist, who uses radiation therapy to treat cancer
- A medical oncologist, who treats cancer with drug therapies.
Surgery is the mainstay of treatment in colon cancer. Preoperative chemoradiation is used in rectal cancer in locally advanced cases. Surgeon can assess the local stage of disease on scans and thus can plan upfront surgery or chemoradiation. Postoperative chemotherapy/radiation therapy is decided after final stage of disease is determined after examining removed specimen.
Robotic Surgery – Cancer, Hernia, Gallbladder Surgery

What is robot-assisted surgery?
Robot-assisted surgery is a type of minimally-invasive surgery completed through small incisions. The da Vinci surgical system uses high-definition, three-dimensional cameras that magnifies image 20 times coupled with specialized surgical tools that enable surgeons to operate with more precision and better control.
The robotic instruments have mechanical wrists that bend and rotate to mimic the movements of the human wrist thus allowing surgeons to make precise movements. Robotic software also negates the effect of surgeons’ hand tremors.
It is an effective minimally invasive alternative to both open surgery and laparoscopy. Surgeons undergo vigorous training with this system before being allowed to use it for surgery on patients. Moreover, there are many inbuilt safety checks in the system that decreases the chances of error. Patients can be rest assured knowing they’ll receive superior surgical care for the best possible outcome.
How robot-assisted surgery works ?
During robotic surgery, your surgeon inserts a tiny camera through a small incision in the surgical area. The camera sends a high-definition, 20 times magnified, 3D image of the surgical site to an external monitor in real-time.
Using computer-assisted technology that guides specialized surgical instruments, your surgeon directs the robot with better control, precision, and range of motion than is possible with traditional surgery. A support team assists the surgeon with other surgical tasks. Thus the use of a robotic system makes difficult steps easier for the surgeon by providing a range of motion and more maneuverability in handling tissue and suturing.
Will the surgeon be with me in the operating room?
Many patients wonder who is operating on them: the robot or the surgeon.
Robot-assisted surgery is a system that enables surgeons to operate with precise, delicate motions by controlling the machine. The robot never makes decisions or performs incisions on its own — it only responds to your surgeon’s hand and finger movements.
Your surgeon is located at a console in the operating room near you and the experienced support staff, directing the procedure the entire time. The robot allows for greater precision than the human hand has on its own, and your surgeon is in charge the whole time.
Conditions that can be treated with robot-assisted surgery
The majority of gastrointestinal issues can be addressed using robotic-assisted minimally invasive surgery, including:
- Appendicitis
- Hernias
- Gallbladder disease and its cancer surgery
- Gastroesophageal reflux disease (GERD)
- Liver surgery
- Surgery of the pancreas including surgery for cancer of the pancreas
- Surgery for the colon and rectum including its cancers
- Surgery for the esophagus, stomach, and intestine
- Gastrointestinal and liver cancer surgery.
The benefits of robotic surgery
Robot-assisted surgery has many benefits. Patients experience these benefits both directly and indirectly. For example, because robot-assisted surgery is minimally invasive, a direct benefit to you is a shorter recovery time. And because the surgeon has better access to the operative area, an indirect benefit is a more precise surgery.
Other benefits include:
- Smaller incisions
- Greater range of motion and dexterity for the surgeon
- High-resolution, the highly-magnified image of the operating field for better visualization during surgery
- Shorter hospital stay
- Lower risk of infection
- Reduced risk of blood loss
- Faster recovery with less pain
- Minimal scarring
- Better clinical outcomes
In addition, due to the enhanced control, flexibility, and precision that robot-assisted surgery offers, surgeons can complete complex or delicate procedures that may be difficult or impossible with traditional surgery.
Am I a candidate for robot-assisted surgery?
Although robotic surgery offers excellent outcomes for many patients, not everyone is a good candidate. The patient is recommended against robot-assisted surgery if:
- You’re unable to have general anesthesia
- You have significant scar tissue or other issues that prevent the cameras from visualizing the surgical area
- You’ve been diagnosed with bleeding problems that put you at risk for surgery
- You’re not a candidate for laparoscopic surgery
After a full evaluation of your condition and overall health, the surgical team in charge will determine if robot-assisted surgery is right for you.
What Are the Advantages of Robotic Surgery Over Laparoscopic Surgery
Robotic surgery is a minimally invasive surgical technique that uses a robotic arm to perform surgery.
The robotic arm is controlled by the surgeon, who sits at a console and uses a joystick to manipulate the arm. This allows the surgeon to perform surgery with greater precision and dexterity than is possible with laparoscopic surgery.
If you are considering robotic surgery, here are some things you can expect:
- You will be given general anesthesia, which will put you to sleep during the surgery.
- The surgeon will make a small incision in your abdomen and insert the robotic arm.
- The surgeon will then use the robotic arm to perform the surgery.
- The surgery will typically take less time than traditional open surgery.
You will likely be able to go home the same day or the next day after the surgery.
Overall, robotic surgery is a minimally invasive surgical technique that offers several advantages over laparoscopic surgery. If you are considering surgery, talk to your doctor about whether robotic surgery is a good option for you.
Advantages of Robotic Surgery
Here are some of the specific advantages of robotic surgery over laparoscopic surgery:
- Improved visualization: Robotic surgery provides the surgeon with a magnified, 3D view of the surgical site. This allows the surgeon to see more clearly and make more precise movements.
- Greater dexterity: The robotic arm has a greater range of motion than the human hand. This allows the surgeon to reach areas that would be difficult or impossible to access with laparoscopic surgery.
- Tremor-free movements: The robotic arm is tremor-free. This means that the surgeon can make very precise movements without the risk of shaking.
As a result of these advantages, robotic surgery has been shown to have several benefits over laparoscopic surgery, including:
- Less pain: Robotic surgery is associated with less pain and a shorter recovery time.
- Lower risk of complications: Robotic surgery is associated with a lower risk of complications.
- Better cosmetic outcome: Robotic surgery is associated with a better cosmetic outcome.
However, it is important to note that robotic surgery is not always the best option for every patient. Some patients may be better suited for laparoscopic surgery or traditional open surgery. It is important to discuss your options with your doctor to determine which type of surgery is right for you.
Myths and Facts About Constipation
Constipation is a common problem affecting people of all age groups. It has many definitions according to people understanding and myths. It is correlated with many symptoms and afflictions. Many problems are attributed to constipation and many homemade remedies are used to get over these problems. Basically we lack understanding of process of passing motion and thus have many wrong notions and myths about passing motion.
“There is no standard when it comes to passing motion. Everyone’s system is different, so if you’re concerned about how many times a day you should pass motion, it really depends on your body. Some people pass motion three to four times per day, others pass it once a week – and they’re fine, not sick. Everything from motion’s consistency (soft or hard) and fecal size, to how long it takes the body to pass feces( stools) is based on the individual. At what time one should pass motion is different for different individual and depends upon his food consumption previous day. What’s important is to your track any changes in bowel habits.”
When is time to consult your healthcare provider is when you notice the following changes in bowel habits:
- Uncomfortable bloating
- Pain while passing stools
- Extremely hard stools, difficult to push out, or thin stools
- Uncontrolled passage of stools, accidents in pants or bed
- Feeling the colon never completely empties
- Pooping, or lack thereof, disrupts day-to-day work and functionality
Passing Gas
It’d be hard to talk about passing of motion without mentioning passage of gas, or as some people call it, farting. Like passing stools, gas is related to bacteria in our digestive system, as well as the foods we eat.
“Gas is a by-product of bacteria in our large intestine digesting leftovers of the foods we ate. Bacteria produce hydrogen, nitrogen, oxygen, carbon dioxide and methane. Yes, it’s the methane that explodes, if you fart near a flame. There is no healthy or unhealthy amount of gas. How much gas you pass and the odor largely depends upon what you have eaten.
Foods that Make You pass stools easily
It’s no surprise that what we eat determines how we pass motion, more or less. Eating foods high in fiber is well known for helping ease time spent on the toilet and producing voluminous, bulky stools, sometimes gas, too.
“Fiber, both soluble and insoluble, holds moisture, keeping stools soft and bulky, which allows the colon to gently squeeze your stools through, as opposed to squeezing and straining to pass small hard bowel movements, possibly with cramping and discomfort.
In addition to what you eat, how much you drink can also play a role.“Staying well-hydrated is important. You know you are well-hydrated if you’re urinating every three to five hours, and the urine is barely yellow. Generally, stools stays softer then, too.
You can try these natural laxatives to ease passage of stools for occasional use:
- Apple juice
- Coconut milk/juice
- Aloe vera juice
- Coffee
- Tea
- Fiber supplements
When is constipation a problem ?
- A sudden and recent change in the routine of passing stools
- Change in color of stool – black color
- Change in consistency and shape of feces
- Blood in stool
- Loss of weight and appetite along with any of the above symptoms
Don’t be scared or shy in discussing these problems with your physicians as they may indicate development of tumor. These symptoms are more important in patients with family history of cancer. They should not cause worry as they are signs for early check up to catch disease at early stage.
Acute Pancreatitis Causes, Symptoms & Treatment
What does pancreas do?
|
What is acute pancreatitis?
Acute pancreatitis is an inflammation of the pancreas that occurs suddenly. It differs from chronic pancreatitis in that there is a discrete episode.
Acute pancreatitis which may be classified as mild, moderate or severe, depending on the amount of damage and organ dysfunction caused by the pancreatitis.
What are causes or risk factor of acute pancreatitis?
Causes of acute pancreatitis are :
- Biliary stones are the cause of 35 to 50 percent of the cases of acute pancreatitis.
- Alcohol intake is the second leading cause of acute pancreatitis.
- Several drugs may cause pancreatitis e.g, immunosuppressants, estrogens, acetaminophen, sulindac. tetracycline, salicylates, erythromycin, pentamidine, thiazide diuretics, furosemide and valproic acid.
- Viral causes include hepatitis A, B, and non-A/non-B; cytomegalovirus; mumps; and coxsackievirus.
- Bacterial causes may include Legionella, mycoplasma and mycobacterium tuberculosis.
- Parasitic infections may also cause acute pancreatitis.
- Pancreas divisum (a congenital defect of the pancreatic ducts).
- Metabolic imbalances (hyperlipidemia and hypercalcemia).
- Sphincter of Oddi dysfunction.
- Scorpion stings.
- Trauma to pancreas may also cause acute pancreatitis.
What are symptoms of acute pancreatitis?
- Upper abdominal pain is main symptom. Usually it is severe and radiates to back.
- Nausea and vomiting are the other most frequent symptoms of acute pancreatitis.
- Fever
- High pulse rate.
- Few patients may have jaundice.
- Patient may have low blood pressure and confusion or coma may occur.
Can acute pancreatitis become chronic pancreatitis?
Yes. Chronic pancreatitis results when inflammation in the pancreas has caused damage and resulted in fibrosis, calcifications and ductal inflammation. It is also possible for patients with chronic pancreatitis to have episodes of acute pancreatitis. Chronic pancreatitis is slow self propagating disease that results in slow destruction of pancreas.
How is acute pancreatitis diagnosed?
Diagnosis of acute pancreatitis is usually made clinically when patient presents with typical pain of pancreatic origin that is pain upper abdomen radiating to back. Further tests helps in confirming diagnosis e.g,
- Increased serum amylase and/or lipase (pancreatic enzymes).
- Ultrasound abdomen
- CT Scan abdomen
Can I prevent acute pancreatitis?
Avoidance of known causes of pancreatitis (i.e., alcohol consumption) may help prevent the onset of the disease. Lifestyle factors such as obesity, alcoholism, hepatitis and others that contribute to a poor state of overall health lead to complications of acute pancreatitis and to a poorer prognosis for recovery.
What is treatment of acute pancreatitis?
The treatment of acute pancreatitis depends on its severity.
- If the disease is considered mild, the patient is usually treated supportively with intravenous fluids, pain control medication, keeping close watch on patient’s general condition so that it does not deteriorates.
- Severe pancreatitis requires close monitoring of the patient to detect possible systemic complications. The patient may be admitted to an intensive care unit. Organisms may reach the pancreas and infect it by crossing the colonic wall. Antibiotics may be used to prevent sepsis. These patients may have some organ failure thus require support for these failed systems.
- Surgical debridement and drainage may be necessary if infected pancreatic necrosis (cell death) arises. CT scan-guided aspiration of necrotic areas may be done to identify the infecting organism so that it may be treated effectively. Surgical intervention is usually done 4 weeks after onset of pancreatitis.
- Therapeutic endoscopic retrograde cholangiopancreatography (ERCP) may be performed in the early stages of acute pancreatitis to remove gallstones and may require sphincterotomy (cutting the sphincter muscle to allow drainage from the biliary/pancreatic tract).
What are possible complications of acute pancreatitis?
Complications can be localized or systemic.
- Systemic complications are usually seen in severe acute pancreatitis. These include
- Low blood pressure
- Lung failure
- Kidney failure
- Inflammation may extend to surrounding organs such as the colon and stomach, gastrointestinal bleeding.
- Localized complications include
- Fluid collections
- Pancreatic pseudocysts
- Pancreatic necrosis
- Pancreatic abscess
Is there hereditary link with acute pancreatitis?
No. There may, however, be genetic influence in chronic pancreatitis.
Liver cancer
Liver cancer is increasing day by day. Its probably due to increase in incidence of cirrhosis of liver that predisposes to liver cancer. Causes of cirrhosis of liver –
1. Alcohol
2. Viral hepatitis’
3. NASH – Non Alcoholic Steatohepatitis
4. Toxins
5. Autoimmune conditions- PBC, Autoimmune Hepatitis etc.
Above are main conditions that cause cirrhosis and predisposes to liver cancer. As the rate of obesity and Diabetes Mellitus is increasing all over world so is the rate of fatty liver and steatohepatitis (injury to liver) that predisposes to cirrhosis and thus liver cancer. So it becomes imperative for allpatients having above mentioned factors to be utmost careful in monitoring the progression of theirdisease to detect cancer at early stage.
FAQs
1. How can liver cancer be prevented?
Liver cancers can be prevented by keeping high risk patients under regular follow
with tumor markers and ultrasound examination. Patient at high risk of getting liver cancers
are mentioned above. So patients with above risk factors who have not progressed to
cirrhosis should be treated according to cause e.g; stopping alcohol, decreasing weight, good
control of diabetes, treating viral hepatitis etc.
2. What is peculiar about liver cancer and its treatment?
Liver cancers usually arise in patients with cirrhosis. This presents peculiar problem
as these patients have damaged liver in addition to tumor. Damaged liver further shrinks
treatment options for such patients. Moreover majority of these patients are unfit for any
form of treatment due to damaged liver. So treatment is tailored according to status of liver
disease and tumour size and location.
3. Is there any medical treatment of liver cancer?
Mainstay of treatment is surgery. Medical treatment is offered to only those cases that
cannot be offered any surgery
4. How can liver cancers be treated?
Best way to treat liver cancer is by surgery. Surgery can be
- Resecting tumor or tumor bearing liver
- Liver transplantation
First option is feasible only in normal livers or in cirrhotic with small tumours. In patients
with cirrhosis best treatment option is liver transplant provided tumor load is within one specific
range. Liver transplantation takes care of diseased liver and tumor simultaneously and thus provides best chances of prolonged life.
In cases of tumor deemed unresectable or patient is unfit for transplant, interventional
radiology provides solution for tumor treatment by
A. Radiofrequency ablation that has same results as surgery in cirrhotics,
B. Tumor chemoembolization
C. Internal tumor radiation by TARE
5. Which specialist is best to treat liver cancer?
Before starting any treatment liver or liver transplant surgeon must be contacted. Liver
surgeon is best person to evaluate patients fitness and tumour resectability and can provide
tailored approach that is best suited for patient’s condition as mentioned above.
Acute and Chronic Pancreatitis Difference and Treatment
What is the difference between acute pancreatitis and chronic pancreatitis?
Acute pancreatitis is an isolated episode of abdominal pain accompanied by elevations
in blood enzyme levels. Essentially, it describes active inflammation of the pancreas.
More than 80 percent of the cases of acute pancreatitis are related to biliary stones or
alcohol use. Acute pancreatitis may lead to chronic pancreatitis.
Chronic pancreatitis is a painful disease of the pancreas in which inflammation has resolved, but with resultant damage to the gland characterized by fibrosis, calcification and ductal inflammation. It is possible for patients with chronic pancreatitis to have episodes of acute pancreatitis.
What causes chronic pancreatitis?
The most common cause of chronic pancreatitis are
- Alcohol consumption.
- Hyperparathyroidism (increased secretion from the parathyroid glands)
- Trauma to the pancreas.
- Tropical pancreatitis, a variant of chronic pancreatitis, is seen in tropical parts of
Asia and Africa, and can affect children between 12 and 15 years of age. - Recurrent acute pancreatitis..
What are the symptoms of chronic pancreatitis?
Symptoms of chronic pancreatitis range widely
- Acute abdominal pain ranging from severe to mild radiating to back. The pain of chronic pancreatitis often radiates to the back, although it may radiate to both upper and lower quadrants. Sitting up and leaning forward may relieve or reduce discomfort
- Vomiting
- Epigastric tenderness
- Weight loss
- Steatorrhea( passing of undigested fat in stools)
- Glucose intolerance/ Diabetes
- Diarrhea which may be chronic (six or more bowel movements per day). The diarrhea is a result of fat malabsorption, which results in bulky, foul-smelling stools that may appear oily and float (steatorrhea).
How is chronic pancreatitis diagnosed?
Chronic pancreatitis is best diagnosed using historical information, serum enzymes,
exocrine function and radiographic studies (X-rays), ultrasound abdomen, CT/MRI scan.
Tests of exocrine function (fat absorption) are helpful.
Are there any particular complications that result from chronic pancreatitis?
Yes. Nutrient malabsorption, diabetes mellitus are main complications of chronic pancreatitis. Patients with chronic pancreatitis are also at increased risk of chronic pancreatitis.
Malabsorption is faulty absorption of nutrients from the digestive tract. In chronic pancreatitis, malabsorption occurs after the capacity for enzyme secretion is reduced by more than 90 percent. Fat absorption suffers to maximum extent in case of chronic pancreatitis.
Chronic pancreatitis affects the endocrine function of the pancreas, responsible for insulin and glucagon production.
Diabetes is common in patients with chronic pancreatitis, and the incidence increases over time with the progression of the disease. Approximately 45 percent of patients with chronic pancreatitis will develop diabetes. Fortunately, the pancreatic form of diabetes is usually mild and the usual complications (retinopathy, nephropathy and vasculopathy) are uncommon. Neuropathic complications may occur with continued alcohol abuse or malnutrition.
How is chronic pancreatitis treated?
Treatment for chronic pancreatitis includes medical, endoscopic and surgical therapy.
Can patients expect long-term relief of pain after surgery?
Surgical intervention provides long-term relief of pain in 90 percent of patients. When
patients have exhausted other avenues of treatment for pain relief, surgery should be
considered.
If I have chronic pancreatitis and am being treated, can I expect a full recovery from this disease?
The changes of chronic pancreatitis are not reversible. However, it is possible to have
control of pain and steatorrhea with medical, endoscopic, percutaneous or surgical
treatment. Surgery provides the best relief of pain in short as well as long term. In
addition to pain relief , surgery can slow down destruction of pancreas thus delaying
onset of diabetes mellitus and malabsoption.

 Book An Appointment
Book An Appointment